The usefulness of non-contact meibography
in diagnosing MGD
What is meibography?
Meibography is a method of morphologically observing the structure of the meibomian glands with transillumination light probe applied to the eyelid. Meibography was first described by Tapie R1 over 30 years ago. The examination was subsequently modified in various ways but it was highly invasive, so it was not adopted for outpatient visits.
Non-contact meibography was developed by Arita et al. in 2008. This technique allows non-contact viewing of the meibomian glands. Non-contact meibography is an objective and highly reliable examination that can be used to diagnose meibomian gland dysfunction (MGD), and this technique has rapidly been adopted around the world.2,3
Development of non-contact meibography
1. Non-contact meibograph attached to a slit-lamp
A CCD camera with an infrared filter (wavelengths of 840 nm or longer) is attached to a slit-lamp.
The biggest advantage of a meibograph(Fig. 1-a) (non-contact meibograph, DC-4 Topcon) attached to a slit-lamp is that meibography can be smoothly incorporated into an outpatient visit.
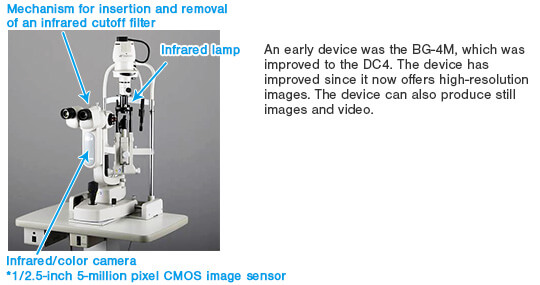
Fig. 1-a: Non-contact meibograph attached to a slit-lamp
After a slit-lamp microscope is used to examine the meibomian gland orifices and lid margins abnormal; i.e. fluorescein staining is performed and ocular surface damage is examined using a blue filter (or a blue cutoff filter). The tear break-up time (BUT) is then measured.
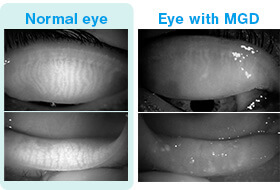
Fig. 1-b: L: Normal eye, R: Eye with MGD
The camera is then fitted with an infrared filter and the upper and lower eyelids are exverted. The meibomian glands are examined and observed on a monitor (Fig. 1-b).
The entire eyelid can examined at a lower magnification to identify abnormalities such as dropout, shortening, cut off, dilatation, or distortion of the meibomian glands. Abnormalities can be examined at a high magnification to examine details like the acini.
2. Mobile non-contact meibograph

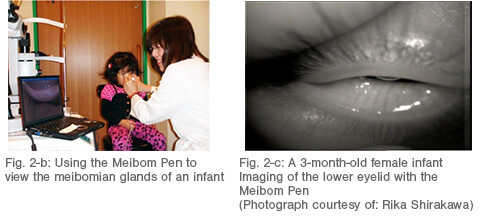
Fig. 2-a: Meibom pen
A meibograph consisting of an infrared LED (wavelength: 940 nm) and CMOS camera.
An advantage of a mobile pen-shaped meibograph (Fig. 2-a)4 (the Meibom Pen, JFC) is that it is truly portable. The meibograph is small enough to fit in one’s pocket and light (120 g) enough that it can be taken on inpatients, used in the operation room, used in screening, or taken on trips abroad. Thus, the meibomian glands can be examined wherever the patient is.
The mobile non-contact meibograph allows examining of the meibomian glands of infants cannot rest their chins on the chinrest of a slit-lamp microscope 5 and of inpatients with a severe systemic illness (Fig. 2-b, 2-c). The mobile meibograph can also be used in the operation room.
3. Keratograph 5M (Oculus)

Fig. 3-a: Keratograph 5M(Oculus)
One of the basic features of the Keratograph 5M (Fig. 3-a) is a corneal topographer, and the Keratograph 5M can also assess the meibomian glands, tear film, and bulbar redness.
The Keratograph 5M provides high-resolution images and can record video (Fig. 3-b).
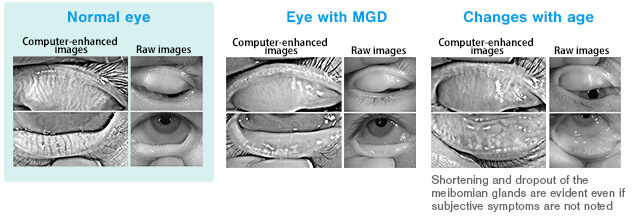
Fig. 3-b: Images from the Keratograph 5M (Photograph courtesy of: Shizuka Koh)
Differences between conventional meibography and non-contact meibography
Conventional meibography uses transilluminating light directly applied to the eyelid and examining the meibomian glands with transmitted light. Thus, the meibomian glands appear dark.
Non-contact meibography uses reflect light of Meibomian gland lipids from the conjunctival side to examine the meibomian glands, so the meibomian glands appear white.
What is examined with non-contact meibography?
White areas in non-contact meibography indicate the autofluorescence of meibum.
Black areas are not filled with meibum, so these areas are where 1. the gland structure has been disrupted and glands have dropped out and 2. areas where the gland structure is intact but keratotic debris has accumulated or areas where the components and amount of meibum have changed or decreased (Nemoto et al., Journal of the Japanese Ophthalmological Society, 2014).
Ocular surface disorders and morphological changes in the meibomian glands
Changes in the morphology of the meibomian glands are evident as a result of contact lens wear, allergic conjunctivitis, or prolonged use of eyedrops to manage glaucoma.
Recently, a multi-center study by the Lid and Meibomian gland Working Group (the LIME Working Group) reported noting changes in the morphology of the meibomian glands of infants with recurrent corneal phlyctenules (Morishige, Suzuki, et al., The LIME Working Group, Journal of the Japanese Ophthalmological Society, 2014). Another study reported that morphological changes in the meibomian glands were a useful way to differentiate sebaceous carcinoma and a chalazion.6
Using non-contact meibography to quantitatively assess the meibomian glands
A meiboscore 2 has been used to semi-quantitatively assess the area of meibomian gland loss. However, the region of the meibomian glands must be assessed quantitatively and in detail in order to assess the meibomian glands before and after treatment.
Arita et al. and Topcon jointly developed software to automatically analyze the region of the meibomian glands depicted by DC-4.7 This software can be used to assess the treatment of MGD with eyedrops, the treatment of MGD with a warm compress (Fig. 4), and the treatment of MGD with oral medication.7,8
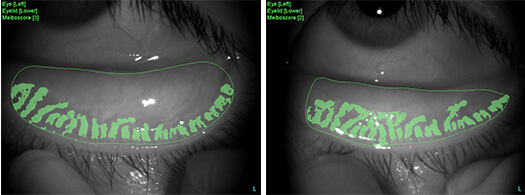
Fig. 4: A comparison of the region of the meibomian glands before and after treatment The regions were depicted with the DC-4 and automatically analyzed with software
The future of meibography
The importance of meibography has been affirmed because of the large number of patients with meibomian gland dysfunction. Unfortunately, however, there is still no “cure” for meibomian gland dysfunction. The pathology of meibomian gland dysfunction has yet to be fully ascertained. If, however, meibomian gland dysfunction is diagnosed and treated early, then the condition can be controlled.
The morphology of the meibomian glands can be viewed objectively and reliably. The effectiveness of treatment can also be determined by quantitatively assessing the region of the meibomian glands. Meibography is a key way to examine the lipid layer as part of the targeted treatment of dry eye (Fig. 5).
In the future, meibography will become a “routine examination” rather than a “special examination” when diagnosing disorders affecting the ocular surface. This will allow early treatment of patients with MGD whose QOL has been markedly diminished.
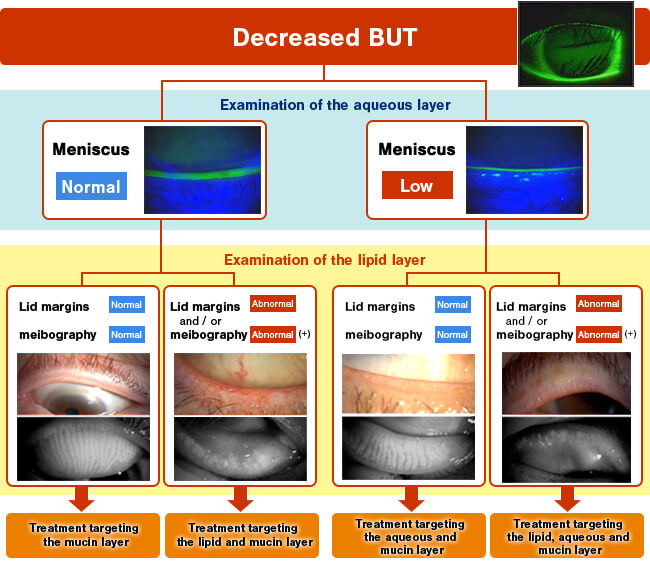
Fig. 5: Examination of the lipid layer for targeted treatment of dry eye
[References]
- 1
- Tapie R. Biomicroscopial study of Meibomian glands (in French). Ann Ocul (Paris):210:637-48,1977
- 2
- Arita R, Itoh K, Inoue K, Amano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology 2008; 115:911-915.
- 3
- Arita R, Itoh K, Maeda S, Maeda K, Furuta A, Fukuoka S, Tomidokoro A, Amano S. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology. 2009 Nov;116(11):2058-63.
- 4
- Arita R, Itoh K, Maeda S, Maeda K, Amano S. A Newly Developed Noninvasive and Mobile Pen-Shaped Meibography System. Cornea. 2012 May 10. [Epub ahead of print]
- 5
- Shirakawa R, Arita R, Amano S. Meibomian gland morphology in Japanese infants, children, and adults observed using a mobile pen-shaped infrared meibography device. Am J Ophthalmol. 2013 Jun;155(6):1099-1103
- 6
- Nemoto Y, Mizota A, Arita R, Sasajima Y. A case with meibomian carcinoma observed in non-invasive meibography. Folia Japonica de Opthalmologica Clinicam 2014;7(3):95-99 [in Japanese].
- 7
- Arita R, Suehiro J, Haraguchi T, Shirakawa R, Tokoro H, Amano S. Objective image analysis of the meibomian gland area. Br J Ophthalmol. 2013 Jun 27. [Epub ahead of print]
- 8
- Arita R, Suehiro J, Haraguchi T, Maeda S, Maeda K, Tokoro H, Amano S. Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol. 2013 Jun;97(6):725-9.