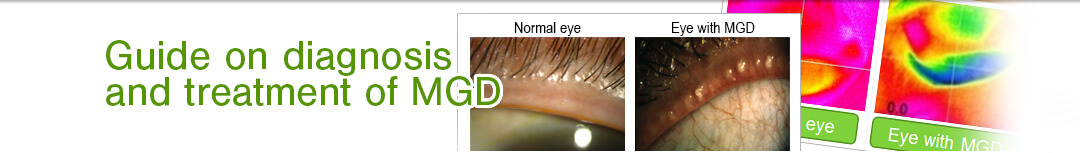
Meibocare and Meibotreatment in Japan
General treatment of MGD
1. Warm compress
Around the world, a warm compress has been reported to be a useful standard treatment for MGD.
Recently, a study indicated that an eye with MGD had palpebral conjunctiva with a significantly lower temperature in comparison to the temperature of palpebral conjunctiva in a normal eye1 and reduced bloodflow in the eyelids. Thus, a warm compress should prove useful.
In an eye with MGD, lipids secreted by the meibomian glands have a higher melting point, so they solidify. A warm compress raises the temperature of the eyelids to the melting point of lipids, so solidified secretions melt. This increases the secretion of those lipids.
Warm compresses are commercially available and include a hot towel, an infrared eyelid heating device (Eye Hot®), and heated eye masks (Hot Eyemask®, Azuki-no-Chikara®, and Memoto Esthe®) (Fig. 1).

Fig. 1: Various warm compresses
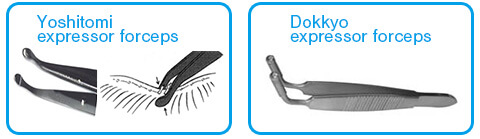
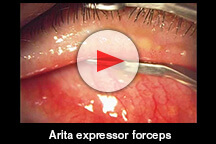
In addition, pressure on the eyelids physically facilitates the secretion of lipids. Medical instruments such as the Yoshitomi, Dokkyo, and Arita expressor forceps (Fig. 2) are used to place pressure on the eyelids. Periodically expressing lipids from the meibomian glands, while causing little pain, should be an effective treatment.
2. Lid hygiene
Lid hygiene should prove effective when performed in conjunction with use of a warm compress.
In the past, the recommended technique was to apply baby shampoo to a cotton swab and wipe the meibomian gland orifices clean. Now, however, cleaning swabs for the meibomian glands and eyelid cleansers are commercially available. These new techniques cause less irritation of the eye compared to the conventional approach. The best practice is to routinely perform lid hygiene twice a day, once in the morning and once at light, much like cleaning one’s face.
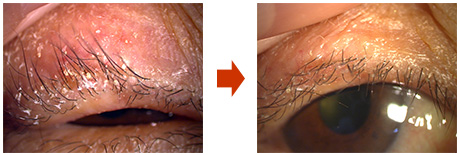
Fig. 3: A case where only lid hygiene was performed for 2 weeks and MGD was alleviated
3. Lipid layer supplementation
Application of a small dose of eye ointment is effective, but if water is absent an oil film will not be formed, so ointment should be applied while also instilling artificial tears.2
Oil-based eyedrops are primarily OTC medications at home and abroad and can be purchased at a pharmacy.
4. Drop therapy
Treatments for dry eye (e.g. artificial tears or hyaluronic acid) are effective treatments for the lipid layer that alleviate subjective and objective symptoms. Recently, a study has reported that the meibomian glands have P2Y2 receptors.3 In the initial stages of MGD when morphological changes have yet to manifest, diquafosol eyedrops can stimulate lipid secretion.
Rebamipide has anti-inflammatory action and anti-oxidant action. Presentations have indicated that instillation of a rebamipide suspension is effective in treating MGD, so this drug may be a future treatment for MGD.
5. Anti-inflammatory therapy
MGD is associated with inflammation of the lid margins, and bacterial flora at the lid margins are associated with inflammation of the lid margins. Meibomian lipids are primarily esters. When bacterial lipase acts on those lipids, fatty acids are freed, causing inflammation of the lid margins.
The ductal epithelium of the meibomian glands is keratinized (hyperkeratinization) and those glands become obstructed. Low-dose steroid eyedrops and antibacterial eyedrops can be used to inhibit inflammation of the lid margins.
A low dose of a tetracycline or a macrolide can be taken for a prolonged period in order to substantially eliminate bacteria from the lid margins and meibomian glands. These antibiotics readily penetrate the tissue of the meibomian glands.
Tetracyclines inhibit the activity of lipase produced by bacteria and macrolides should have additional anti-inflammatory action.
6. Diet therapy
A study has indicated that consuming foods and supplements with a large amount of omega-3 fatty acids is effective in treating MGD 5, but detailed studies have yet to be conducted.
[References]
- 1.
- Arita R, Shirakawa R, Maeda S, Yamaguchi M, Ohashi Y, Amano S.Decreased surface temperature of tarsal conjunctiva in patients with meibomian gland dysfunction. JAMA Ophthalmol. 2013 Jun 1;131(6):818-9
- 2.
- Goto E, Shimazaki J, Monden Y, et al. Low-concentration homogenized castor oil eye drops for noninflamed obstructive meibomian gland dysfunction. Ophthalmology 2002;109:2030-2035.
- 3.
- Arita R, Suehiro J, Haraguchi T, Maeda S, Maeda K, Tokoro H, Amano S.Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol. 2013 Jun;97(6):725-9
- 4.
- Suzuki T, Mitsuishi Y, Sano Y, Yokoi N, Kinoshita S. Phlyctenular keratitis associated with meibomitis in young patients. .Am J Ophthalmol. 2005 Jul;140(1):77-82.
- 5.
- Macsai MS. The role of omega-3 dietary supplementation in blepharitis and meibomian gland dysfunction. Trans Am Ophthalmol Soc 2008;106:336-356.